Diabetes can affect multiple systems in the body, but its impact on the lower limbs is among the most serious and often overlooked. When circulation to the feet becomes critically compromised, specialised vascular intervention may be required to prevent further deterioration and protect limb function.
In this blog, we explain how diabetes affects foot circulation, recognise warning signs, and understand when surgical intervention becomes necessary.
Understanding Diabetic Foot Conditions
Long-standing diabetes often leads to structural and functional changes in the blood vessels and nerves supplying the feet. Poor circulation limits oxygen delivery to tissues, while nerve damage reduces sensation, allowing minor injuries to go unnoticed. Over time, these factors combine to create complex foot conditions that require prompt medical attention. Patients commonly experience diabetic foot symptoms such as numbness, tingling, slow-healing wounds, skin colour changes, or persistent pain during walking or rest.
As the condition progresses, everyday foot care becomes increasingly important for individuals with diabetic feet. Without early intervention, circulation problems can worsen, leading to ulcers, infections, and tissue damage.
Causes and Progression of Diabetic Foot Problems
Diabetic foot problems usually develop gradually and result from multiple interconnected factors related to long-term diabetes.
The most common causes of diabetic foot progression include the following:
- Poor blood sugar control leading to damage to small and large blood vessels
- Peripheral arterial disease reduces blood flow to the lower limbs.
- Nerve damage that diminishes pain sensation and injury awareness
- Repeated minor trauma caused by ill-fitting footwear or pressure points
- Delayed wound healing and increased susceptibility to infection
Over time, this progression can result in serious diabetic foot problems, including tissue death and infection, making early vascular evaluation essential for limb preservation.
Role of Vascular Surgery in Diabetic Foot Care
Vascular intervention is required if there is inadequate circulation to the affected foot despite traditional treatment. At this point, a structured surgical approach aims to enhance blood circulation and tissue healing.
- The main goals of vascular surgery in diabetic foot are:
- Restoring blood supply to the tissues deprived of oxygen.
- Healing chronic ulcers and wounds.
- Reducing the risk of amputation and infection.
- Enhancing movement and the quality of life.
- Long-term foot preservation in terminal illness.
Types of Vascular Surgery for Diabetic Foot
The choice from the available vascular surgery types depends on the location and severity of arterial blockages, overall health status, and wound condition. Before selecting a procedure, a detailed vascular assessment is performed to determine the most effective method for restoring circulation.
The commonly used types of vascular surgery for diabetic foot management include the following:
- Angioplasty to widen narrowed or blocked arteries
- Stent placement to keep blood vessels open after angioplasty
- Bypass surgery to reroute blood flow around blocked arteries
- Thromboendarterectomy to remove plaque from arterial walls
An individualised approach ensures that the chosen method supports wound healing, reduces complications, and aligns with the patient’s long-term vascular health needs.
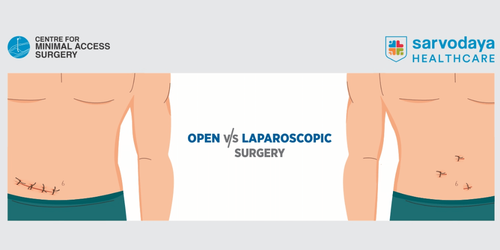
Endovascular and Open Surgical Approaches
Modern diabetes foot care incorporates both minimally invasive and open surgical techniques, depending on disease complexity. The vascular specialist doctor carefully evaluates which approach offers the safest and most durable outcome.
The two main approaches to diabetic foot vascular surgery are outlined below for clarity:
- Endovascular procedures, performed by an experienced endovascular surgeon, involve catheter-based techniques such as balloon angioplasty and stenting. These methods are less invasive, offer quicker recovery, and are often suitable for high-risk patients.
- Open vascular procedures involve surgical bypass or arterial repair and are recommended when blockages are extensive or unsuitable for minimally invasive treatment. These procedures provide long-term improvements in circulation in advanced disease.
Both approaches are integral to comprehensive vascular surgery care. Selection is guided by diagnostic findings, limb viability, and overall patient health, ensuring the best possible functional and clinical outcome.
Read More- Diabetic Retinopathy - Most Common Eye Problem In Diabetes
Preoperative Assessment and Diagnosis
Before proceeding with diabetic foot vascular surgery, a thorough clinical and diagnostic evaluation is essential to determine disease severity and surgical suitability. This assessment helps identify arterial blockages, tissue viability, and associated medical risks.
A structured preoperative work-up typically includes the following components:
- Detailed medical history and physical examination of diabetic feet
- Vascular imaging, such as Doppler ultrasound, CT angiography, or MR angiography
- Assessment of wound extent, infection status, and tissue perfusion
- Evaluation of cardiac and renal function to minimise surgical risk
This comprehensive approach allows a vascular surgeon in Faridabad to design a personalised treatment plan.
Recovery and Post-Surgical Care
Post-operative care is carefully monitored to ensure circulation improves steadily and complications are avoided.
Key elements of recovery include the following:
- Regular wound inspections and dressing changes
- Blood sugar optimisation to support tissue healing
- Medication management to prevent clot formation
- Gradual mobilisation under medical supervision
- Ongoing foot care education and monitoring
Healing timelines vary depending on the procedure performed and individual health factors. With appropriate follow-up and lifestyle modifications, vascular surgery significantly improves limb survival and quality of life for patients undergoing diabetic foot vascular surgery.
Read More- 7 Day Indian Diet Plan for Diabetic Patients
Preventive Strategies and Long-Term Foot Care
Long-term success following treatment depends heavily on preventive care and ongoing monitoring.
Key preventive strategies include the following:
- Daily inspection of feet to identify early diabetic foot symptoms
- Use of appropriate footwear to reduce pressure and prevent injury
- Strict blood sugar control to slow vascular damage
- Regular podiatry and vascular check-ups
- Prompt medical attention for cuts, ulcers, or skin changes
Conclusion
With advances in diabetic foot vascular surgery, many patients can achieve improved circulation, wound healing, and limb preservation through a structured, multidisciplinary approach.
Sarvodaya Hospital, Faridabad, offers comprehensive care for patients requiring vascular surgery for diabetic foot, supported by advanced diagnostics, experienced surgeons, and coordinated diabetes management. The hospital’s integrated model allows a vascular surgeon in Delhi NCR to work closely with wound care and diabetes teams.
Patients are encouraged to seek expert guidance and book an appointment now to take proactive steps towards effective diabetic foot management.